Review
Fast Facts
- Septicemia is the most expensive medical condition treated in U.S. hospitals nationwide by a significant margin. Ranking well behind are osteoarthritis, liveborn, complication of implant/device/graft and acute MI, according to the Agency for Healthcare Research and Quality.
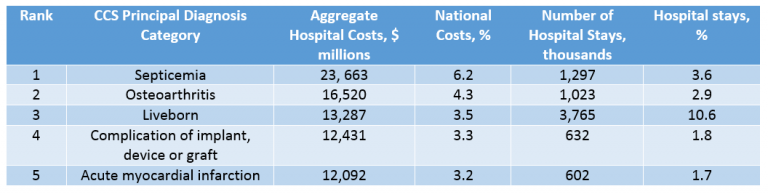
- Septicemia is the No. 1 cause of inpatient mortality nationwide.
- Overall in-hospital death rates have declined, but have increased 17% for septicemia, according to the CDC.
- Noted in research by the Sepsis Alliance, the risk of death increases significantly, at an estimated 8% per hour, with delay in appropriate identification and treatment.
- Approximately 80% of deaths caused by sepsis could be prevented with rapid diagnosis and treatment. [1]
Recent Findings from 2017
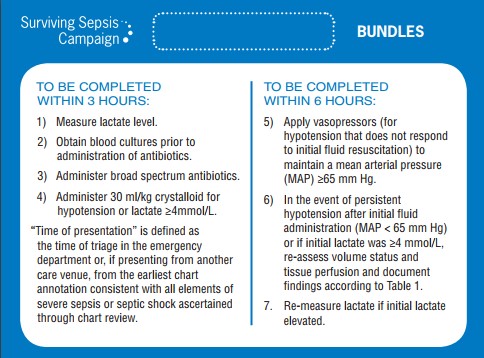
- According to a study published in the New England Journal of Medicine from patients in New York, a longer time to completion of the three-hour bundle of care resulted in increased in-hospital mortality.
- According to research published in JAMA from the Nationwide Readmission Database, sepsis accounts for more readmissions, with a higher cost per readmission than any of the four conditions CMS tracks for reimbursement purposes. The conditions include: heart attack, heart failure, chronic obstructive pulmonary disease and pneumonia.
- An education program that helps with the identification, treatment and management of sepsis implemented in coordination with rapid response teams can result in significant reduction in sepsis related deaths, according to a study published in the Journal of Critical Care.
Challenges
Challenges with sepsis occur at many different levels. At the hospital and system level, repeat lactic acid testing is a common challenge. For physicians, accepting the concept that IV fluids benefit all patients in septic shock, including those patients with CHF and renal failure, where we typically limit fluids is a challenge. From a department perspective, rapid identification of septic patients poses challenges. Unlike conditions that tend to be more obvious such as trauma, acute MI and stroke, these patients may present in a more subtle manner. Developing a systemized approach across multiple departments is essential. With a time-sensitive condition such as sepsis, a set algorithm leads to improved patient outcomes. But even with such systems, compliance with treatment still has quite a bit of room for improvement. According to Dr. Sean Townsend, intensivist and researcher, even the best-performing hospitals with systematic methods to identify and treat sepsis comply with all elements of the sepsis bundles only 60 to 70% of the time, despite the widespread focus on sepsis.[2]
Best Practices
Like most hospitals and health systems, ApolloMD has focused on the identification, treatment and management of sepsis within our partner hospitals. Some of the best practices that we have implemented with our partners:
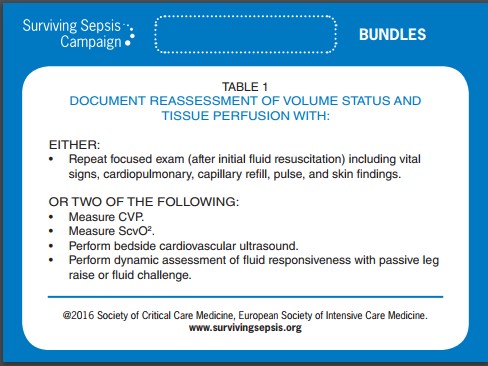
Establish specific order sets within the EMR systems to include the 3-hour bundle, 6-hour bundle and appropriate antibiotics.
While the 3 and 6 hour bundles are common to all hospitals, the antibiotics may differ slightly from one facility to the next based on resistances patterns of organisms in the community, and the formulary of a particular hospital. Another suggestion, and one that has produced great results at our partner facilities CHS Blue Ridge Morganton and Valdese, is establishing Diagnostic Order Sets and Resuscitative Order Sets. These are used in conjunction with the Sepsis Order Sets and allow further efficiency of workup and more consistency in patient care.
Announce sepsis codes.
Just as codes are announced for trauma, stroke, heart attack and other time-sensitive conditions, “Code Sepsis” places immediate awareness on a particular patient. All team members including lab, radiology, nursing, and physician have a coordinated immediate focus on meeting the rapid treatment goals associated with sepsis.
Establish Sepsis Champions within the ED teams.
Sepsis Champions were implemented across all ten of our WellStar Health System partner facilities. Each champion tracks sepsis data and provides rapid feedback to each team member, with positive feedback to individual providers and any opportunities for improvement. The rapid feedback has led to great strides and improvement in the EDs across the system.
New research is constantly developing on the care and management of sepsis in the ED. Use these resources to learn more:





